The FQHC Telehealth Consortium Telehealth Playbook is a “how to” guide to support the adoption and sustainability of telehealth at health centers. Like telehealth, it is evolving, seeking to incorporate “best practices” and tools as they become available. It consists of the following chapters:
- Introduction
- Strategy & Leadership
- Clinical Integration
- People
- Technology & Tools
- Reimbursement & Policy
Each chapter includes the overall strategy and approach to improving telehealth performance, as well as supplementary documents and resources.
Notice: This Playbook should not be considered legal advice and should be adapted for each community health center, based on the needs of the population and updates to federal, state, and local policies. The materials are intended for informational purposes only.
Telehealth Definition
The term “telehealth” includes telemedicine services but encompasses a broader scope of remote health care services. Telehealth is the use of electronic information and telecommunications technologies to support patient care through remote clinical and non-clinical audio and video services, patient and professional health-related training and education, mobile health applications, asynchronous communication via patient portals and text messaging, and home-monitoring/self-care digital communication technologies.
It can be used as a complement to in-person care delivery when clinically appropriate and when a patient has access to broadband, a device such as a phone or computer, and education on how to use telehealth modalities to support their health and wellness.
Improvement Approach
The FQHC Telehealth Consortium has developed a long term strategy in the form of a Maturity Model, which demonstrates the capabilities needed to advance telehealth performance. The model represents “what” we hope to achieve.
The Consortium has also created a Driver Diagram, which demonstrates the key drivers needed to advance performance. The diagram represents “how” to improve performance, and it will be updated as Consortium health centers continue to test the drivers and identify new drivers.
Maturity Model
In general, a maturity model is a tool used to demonstrate capabilities needed to achieve improved levels of performance, in a holistic manner. The model is the basis for assessing each health center’s telehealth strengths and opportunities.
The Consortium Maturity Model provides high-level guidance for advancing telehealth capabilities. It answers the question, “Where should we go (or where could we go) in building sustainable and equitable telehealth at the health center?”
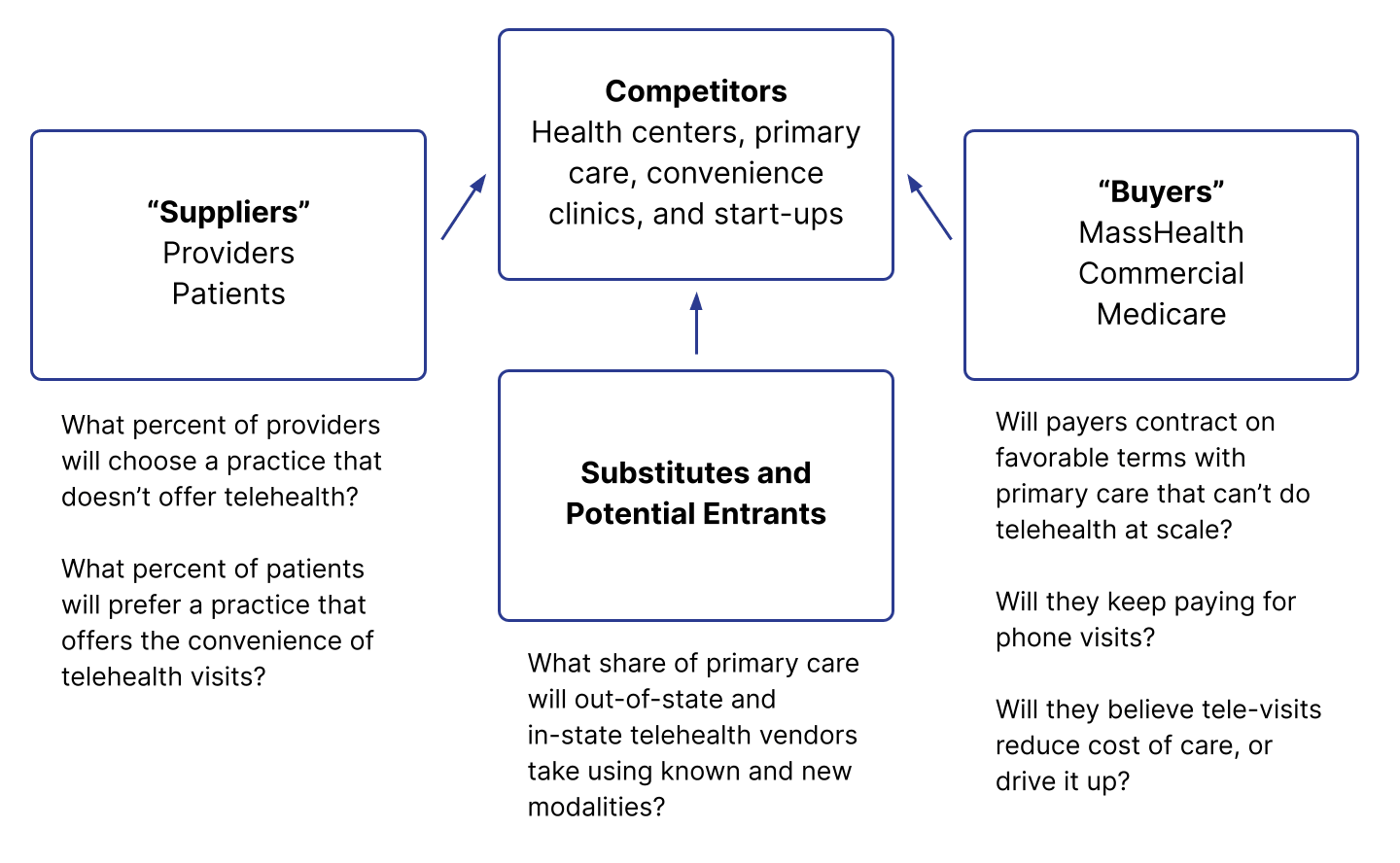
Long-Term Value to Suppliers and Buyers
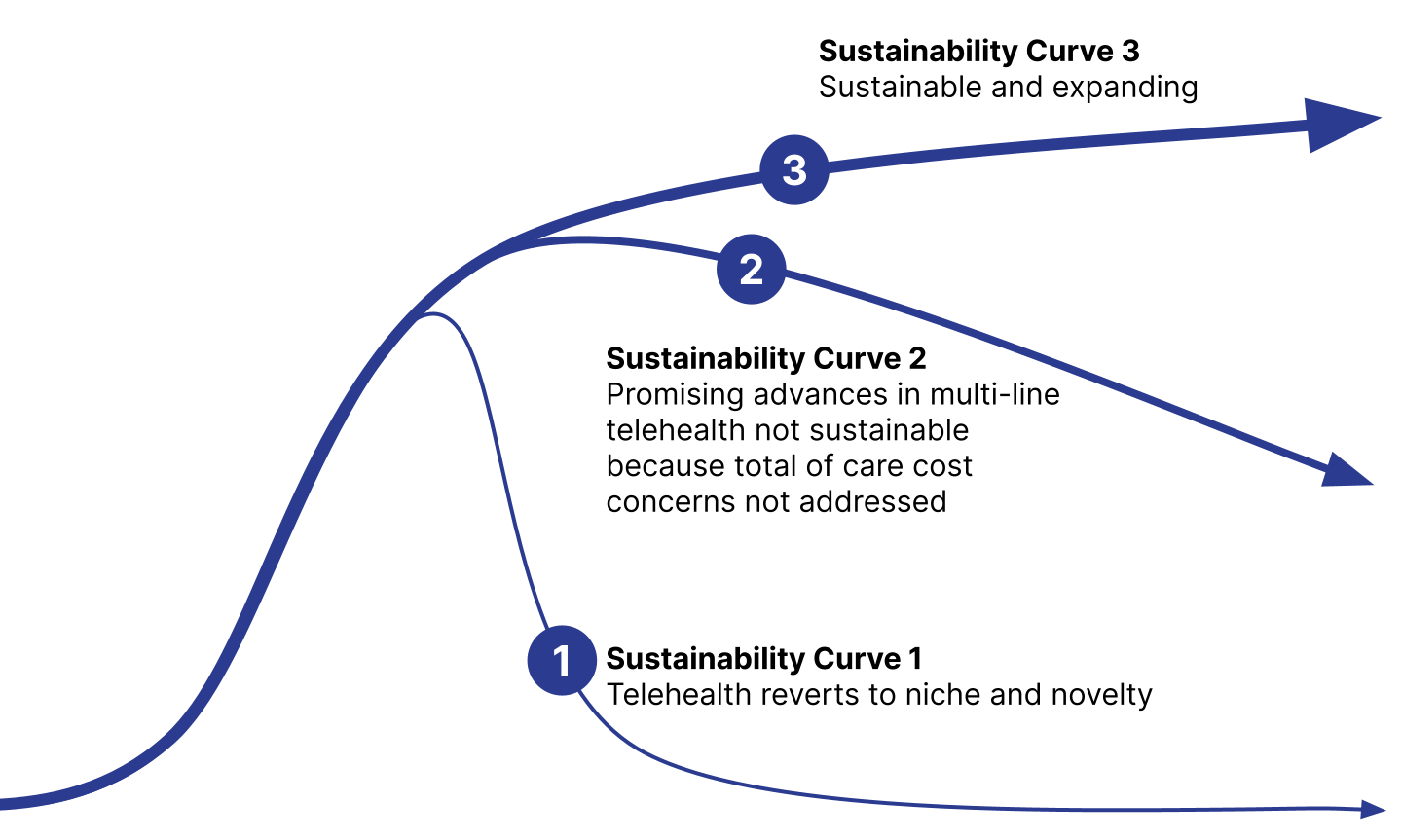
This framework is Michael Porter’s Five Forces approach to understanding the nature and intensity of industry competition. We utilized this approach in discussions with health center senior leaders in Spring 2020 as a tool to develop a sustainable, long-term strategy for telehealth. The curves diagram below illustrates potential trajectories for telehealth and is the basis for the dynamic levels, or “curves” in the Maturity Model.
Sustainability – Which Curve Will We Be On?
Telehealth Consortium Maturity Model
| Curve 1: Covid-19 Response | Curve 2: Care integration | Curve 3: expansion & Sustainability | |
|---|---|---|---|
| Strategy & Leadership | All-consuming focus; critical to patient care and revenue needed to survive | CEO and entire C-suite champions the change; integrated in strategy, budget, and execution | Telehealth embedded in health center clinical models; drives financial, quality, and health equity goals |
| Clinical Integration | COVID and non-COVID workflows; telehealth substitutes for some in-person visits to health center | Integrated into delivery of care across all health center disciplines and for all patients | On-site and virtual specialty care integration; optimization of community-based care with remote monitoring, in-home testing, and portal use |
| People | Rapid adoption of phone/video visits by health centers; variability in digital access for patients | Care teams competent in using telehealth for patient care and engaged in ongoing innovation; all patients able to access telehealth modalities | Providers routinely utilize access to specialty consults; patients engage in tech-enabled community-based care |
| Technology & Tools | Rapid deployment for phone visits; some video | EHR-integrated, HIPAA-compliant, video-enabled; patient devices, data plans, and remote monitoring deployed | Specialists integrated through eConsults and synchronous patient visits |
| Reimbursement & Policy | Liberal to support COVID-19 delivery of care | FFS reimbursement supports phone and video; partial patient enablement support; HRSA, FTCA, other regulatory flexibilities | Sustainable reimbursement HRSA modernization |
Equity Framework
The Telehealth Equity Framework is intended to drive and guide efforts to integrate and maintain equitable telehealth practices at health centers through ongoing and iterative application. Designed in collaboration with Health Resources in Action, the framework aligns with and expands upon the Maturity Model by identifying equity drivers and practices for each domain of the model.
Telehealth Equity Framework
| Domains | Equity Drivers | Equitable Telehealth |
|---|---|---|
| Strategy & Leadership | Practice collective reviews of telehealth policies to prevent “gatekeeping” Establish Board telehealth sub-committee Create opportunities for community to share decision making about telehealth | Equity and community input are embedded in and drive health center strategy decision-making for telehealth care delivery |
| Clinical Integration | Understand what the access points are for telehealth and allow for patients to utilize any access points Integrate fields in clinical systems to document patient choices/preferences and needs for telehealth care; regularly confirm/update this information | Patient choice and needs drive decisions regarding the mechanism(s) of their telehealth care; virtual supports to address needs are embedded in clinical systems and do not need to be requested |
| People | Intentionally engage people in the community in telehealth decision-making Deploy telehealth navigators to access patient digital access and provide support Measure who is and who is not accessing telehealth services and why | Providers have cultural awareness/competency/humility in providing care to their patients and adapt telehealth care delivery to align with patient needs |
| Technology & Tools | Intentionally create and actively engage in partnerships with community organizations that promote technology and those that enable access Partner with vendors who are committed to and experienced in working with diverse populations (e.g., language needs, tech literacy) | Technology is structured to enable flexibility/be responsive to patient choice, provide needed support(s), and ease/facilitate engagement in telehealth |
| Reimbursement & Policy | Collect accurate data that is representative of the patient populations being served to identify who is and is not able to access telehealth Monitor closely the developments in industry, policy, and reimbursement that will or may impact equity and/or telehealth goals | Policies directly identify equity as a priority and these priorities, as well as related date, drive telehealth policy decisions; telehealth advocacy efforts are informed by equity priorities/data and community input |
Driver Diagram
A driver diagram is a performance improvement tool used to visualize all the factors that contribute to the achievement of an initiative’s aim (goal). It maps the theory of change, from the aim statement to the primary drivers of what contribute directly to achieving the aim, and then to the secondary drivers that represent specific tactics that support the primary drivers.
Our Telehealth Driver Diagram demonstrates the key components needed to advance performance, and answers the question, “How will we mature our telehealth capabilities?” The diagram aligns the primary drivers with the Maturity Model domains and includes secondary drivers that provide guidance for testing out new approaches of delivering virtual care. Our diagram will be updated as Consortium health centers continue to test improvement ideas and identify new tactics for adopting and sustaining telehealth.
-
Partner Resource
Telehealth Consortium Driver Diagram
Develop a sustainable, patient-centered, and equitable telehealth model and achieve an advanced level of maturity at Consortium FQHCs
PDF ↓
Primary & Secondary Drivers of Success
Strategy & Leadership
- Board of Directors engagement
- Designated Team: Executive Sponsor, Provider Champion, Support Staff
- Virtual care built into health center budget
- Established measures of success
- Maturity Model assessment, gap analysis, and improvement plan
Clinical Integration
- Redesigned care team roles
- Scheduling guidelines and workflows for virtual visits
- Clinical pathways for virtual care and hybrid models
- eConsults for specialty referrals
People
- Provider & staff training
- Patient education
- Digital equity
- Satisfaction/Engagement surveys: patients, staff, providers
Technology & Tools
- Telehealth platform, integrated with EHR
- Accessibility to smart phones and data plans for patients
- Remote patient monitoring
Reimbursement & Policy
- Expanded reimbursement guidelines at state and federal levels
- Advocacy for HRSA and other regulatory agencies to support sustainability
FQHC Telehealth Consortium Members
FQHC Telehealth Consortium members serve over 700,000 patients from 35 locations across Massachusetts. See our full list of members.

What Patients Prefer about Telehealth
“It was faster, my child had allergies and I sent a photo to the provider and they sent me my prescription the same day.”
“Since I don’t have a car, it’s better for me to have the encounter with the provider by phone. If I have any kind of worry or doubt about my baby, I can simply call the center. They have always answered kindly.”
“For me, I do not have transportation. Since losing MassHealth (and their ride assistance), being able to make appointments that someone can take me to is VERY difficult.”
“I like it better because my job is very demanding. I work 5 to 5 every day so telehealth makes it easier… I can step aside for 15 minutes and take the call.”
Acknowledgements
The FQHC Consortium was established to create a robust and sustainable telehealth platform to support high-quality, team-based primary care to improve health, reduce disparities, and provide a national telehealth model for under-resourced populations. It is a collaboration of 35 Federally Qualified Health Centers (FQHC’s) led by:
- Community Care Cooperative (C3), a 501(c)(3) non-profit, Accountable Care Organization (ACO) governed by Federally Quality Health Centers (FQHCs). Our mission is to leverage the collective strengths of FQHCs to improve the health and wellness of the people we serve. We are a fast-growing organization founded in 2016 with 9 health centers and now serving hundreds of thousands of beneficiaries who receive primary care at health centers and independent practices across seven states. We are an innovative organization developing new partnerships and programs to improve the health of members and communities, and to strengthen our health center partners.
- Massachusetts League of Community Health Centers (League), a Primary Care Association (PCA) that promotes population health equity for all through leadership and programs supporting community health centers in achieving their goals of accessible, quality, comprehensive, and community responsive health care
Funding
Funding for the Phase 1 Initiative of the Consortium was made possible by sources of C3 and League funding, as well as generous support from:
- Barbara and Amos Hostetter
- Beacon Health Options
- CareQuest Institute for Oral Health
- Gordon and Betty Moore Foundation
- Harvard Pilgrim Health Care Foundation
- Federal Communications Commission administered COVID-19 Telehealth Program funded by the CARES Act
- Landry Family Foundation
- Massachusetts Broadband Institute
- Massachusetts Executive Office of Health and Human Services
- The Digital Equity Fund of the Essex County Community Foundation
- The Klarman Family Foundation
- The Patrick J. McGovern Foundation
- The Paul and Phyllis Fireman Charitable Foundation
- UnitedHealthcare Community Plan of Massachusetts